UCR 19: FAQs - Can CPT code 50386 be done in the office? Can I bill CPT 55700 with 76872, 76942, 96372 & J1580?
August 24, 2020
Mark, Ray and Scott answer 3 questions from the Urology Coding and Reimbursement Group
- Can CPT code 50386 be done in the office? The provider wants to remove the stents without cysto whenever possible as he says it is more comfortable for the pt and less risk of infection. Does this still need ultrasound guidance to do in the office? Haven't done one of these before in the office. Please advise. Thank you.
- Good morning, new to ASC billing for my Urologist. My doctor performed a TRUS/BX at an ASC and I am billing the facility charge. For the facility, can I bill CPT 55700 with 76872, 76942, 96372 & J1580. I have searched on line but unable to find anything relevant. Please advise
- Help please.
Pt had gross hematuria and BPH. Would CPT 52214 be correct or 52601-52?....the resectoscope has me questioning my code choice..... "...........cystoscope was removed and a 26Fr resectoscope was inserted. Using the bipolar rollerball the entire prostatic fossa was fulgurated. Hemostasis was attained. The resectoscope was removed and a 20fr 3-way catheter was inserted." Doc said TURP but think I'd need him to re-phrase his op note.....no?
Thank you
Upcoming E&M 2021 Live Online Workshops
Learn More
Dates (all times Eastern)
September 18, 2020 - 5:00 pm
September 26, 2020 - 10:00 am
October 8, 2020 - 6:00 pm
October 28, 2020 - 5:00 pm
E&M 2021 Preparation Checklist
Join the discussion:
Urology Coding and Reimbursement Group - Join for free and ask your questions, and share your wisdom.
Click Here to Start Your Free Trial of AUACodingToday.com
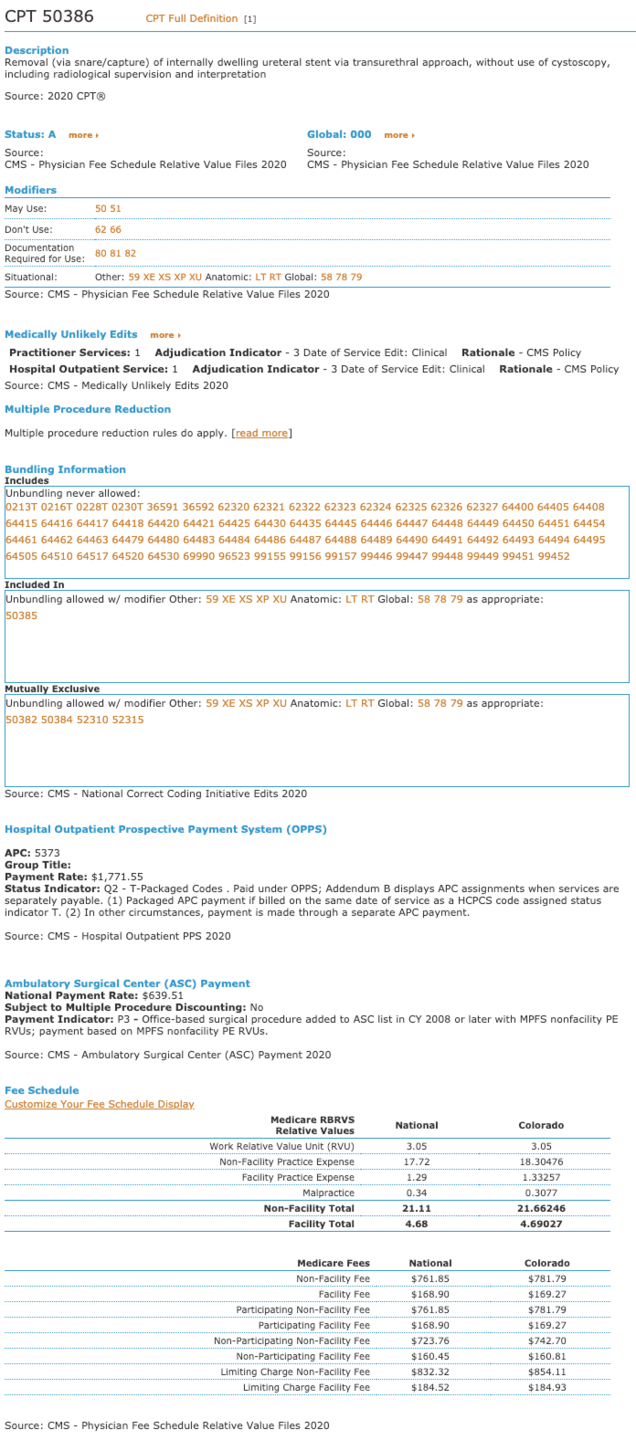
Screenshot: CPT Code 50386 from AUACodingToday.com
Transcript
Scott 0:00
Welcome to the urology coding and reimbursement Podcast, where we help urologist and staff achieve economic and practice efficiency. So there is time and energy, focus on patient care, and a happy life. I'm your host, Scott painter with my co hosts, Mark painter and Dr. Ray Painter.
Welcome to Episode 19 of Urology coding and reimbursement podcast. I'm your host, Scott painter with my co host, Mark painter and Dr. Ray Painter, and today we're going to do some frequently asked questions, or go on to the urology coding and reimbursement group, which you can find and join for free on prs network COMM And today, we have three questions that we're going to answer. The first one is from Lisa and Lisa asks, Can CPT code 50386 be done in the office? That provider wants to remove the stance without Cisco whenever possible, and he says it's more comfortable for
predict patient and less risk of infection. Does this still need ultrasonic guidance to do in the office? I haven't done one of these before, please advise. Thank you.
So turn it over to Mark and Ray. Okay, so the code if you look up on coding today 50386
Mark 1:22
has a couple of things that would indicate that yes, this is an allowable service to be provided in the office. The first place that we check is the practice expense values to see if there is a non facility practice expense. And if we have one, is it different from the facility practice expense, so in this case, and really it should be higher and in every case, so that is that is true in this case, so 50386
does look like it would be paid for in the office setting. So I don't see Any problems with that? Obviously, the doctor has to feel that he is comfortable in doing this. And it meets all the medical necessity and safety guidelines. So as long as he finds he or she find that they can do this in the office that certainly allowed and you can see it's a significantly higher payment in the office setting at a national average of 761 85 as opposed to doing it in the the ASC or the hospital which the national unadjusted fee is 168 90. So a significant difference there. And I noticed you asked about maybe requiring the ultrasound. The description does say including radiologic, supervision and interpretation which means you can't bill separately for it but it does not say Say it is required from the CPT disc description. So, in that instance relative to requiring the use of an ultrasound, that is a clinical call that the physician can make whether or not they need that radiologic supervision, obviously looking at the, the facility or excuse me, the non facility practice expense our views, they are built in cluding that So, from that standpoint, they do think it is common to be used in that particular instance. But as far as, you know, ultimately telling the physician out of practice that is not something that is absolutely required within the billing framework. So, that might be something that you look at from the clinical side. So, hopefully that gives you the answer there. Go ahead and charge the 50386 in the office setting if you feel it's safe and effective.
Scott 4:04
And we'll go ahead and put up a screenshot of the 50386 from a coding today on the podcast website and also will refer to it down below the question as well on the urology coding and reimbursement group. So also that is prs network comm forward slash 019 for podcast episode 19 re did you have something in?
Ray 4:32
Yeah, Mark, if that'd be the case just looking at it. Why can't I just tie a string on the the stent or use a stent with a string and I would be removing it in the office and certainly I would need an ultrasound to do that.
Mark 4:52
So, they it is the removal via via snare or capture which parenthetical of an internally dwelling ureteral stent via transurethral approach. So you do need to look at the full description there. We're assuming based on the question that they are using stent, removal from a capture or snare, not just the string. So, that's really not billable from the string side of things as we've seen across the board so it can't have a string and you're not doing a grasper and pulling it out. You are using really a probably a ureteral catheter to go up there and snag that.
Ray 5:46
Thanks for clarifying. I just didn't want other people to get into troubles, start removing stents and charging this code.
Mark 5:54
Yeah. Good. Good capture. All right. Okay. So
Scott 6:01
that answers that question for the next question we have from Roseanne. Good morning New Day ASC billing for my urologist. My doctor performed a transurethral ultrasound biopsy at an ASC and I am billing the facility charge for the facility. Can I bill? CPT 557 hundred with 768727694293796372 and j 1580. I've searched online but I'm unable to find anything, please advise.
Mark 6:39
Okay, so Roseanne? Good question. And yeah, the facility is a little bit different as to how you can report from as far as a coding standpoint, it is based on the procedures that you provide. So, the 55 700 is an appropriate code for the ASC and the seven In 6872, is actually if you look on the ASC payment agenda, which you can find up at the at CMS, or you can find located in least the information, for the most part is in coding today under the ASC payment. So the 76872 is as designated as a code that can be reported separately, even if it's integral to the procedure. So you can build a 55 700 you can build a 76872. Now the 76942 is bundled in Medicare, and unbundling can never be allowed. And actually, it's set up as a mutually exclusive code, which means typically, if you pay five or if you charge the 76872, and the 76942 on the Same claim, they'll actually pay you the lessor. Now this is from the professional side the 76942 instead of the 76872. So you do want to be careful, even on the professional side. On the ASC side, the 76942 is considered to be a package service and is never paid from Medicare's perspective. So, you'll find that with a lot of the private payers, they'll find the same. So right now, you're still at 55 707 687 to now drugs and injections and all of that is part of the facility fee. So the 96372 and the J 1580. are also not billable from the ASC. So, in the end, what you're left with for a prostate needle biopsy is the 55 700 and the 76872. If you have the appropriate documentation for the physician diagnostic transurethral ultrasound. So which really, by hopefully you remember on the professional side does require documentation, like a little radiology report in addition to the prosthetic needle biopsy itself. So you want to be careful that the documentation matches everything that you're doing. And then, of course, the other thing from the facility side. I don't know if you're still billing for your urologist. But when you build the 55 700 and the 76872, you would need to add a 26 modifier to the 76872. The code 96372 and 76942 and j 1580. should not be billed by the physician to Medicare. If you have a plan that is still paying both the 76872 and the 76942 you will also need to add the 26 modifier to the physicians bill on the 76942. So, just to kind of recap, you know, ultimately if you're billing Medicare, your physician would bill a 55 700 and a 76872 dash 26 the facility or the ASC would bill up 55 707 6872.
Scott 10:27
All right, anything to add on that Ray?
Ray 10:30
No, I was just going to mention mark that you mentioned the 26 modifier for the professional and made it clear that you do not need to put the TC modifier on when you're in the ASC as you would in the office.
Mark 10:48
Correct, right.
Scott 10:52
All right.
Okay, let's go on to the next one. Last question for today. We've got a question from Linda. And Linda says help please. patient had gross hematuria and BPH. Would CPT 52214 be correct, or five to 601 dash 52. The resectoscope has me questioning my code Joyce says the scope was removed and a 26 French red resectoscope was inserted. Using the bipolar rollerball the entire prostate fascia was full grated. He must stasia was attained the red dress their sex scope was removed and a 20 French threeway catheter was inserted in quotes and then it says doc said to you RP, but think I need him to rephrase his note.
Mark 11:48
No, so yeah, I would. So I would agree. I mean, there is a possibility given what you've said that they the patient had gross hematuria and BP Ah that they are potentially providing or doing a tarp I mean that is a treatment for the BPH but given the the verbiage that you included here, it really looks like it was fitting for five to to one four and the 52214 reads says do you ask me with full duration of trikon bladder neck prosthetic fossa urethra, or Peri urethral glands. Now, given what it kind of says there, it looks like they just did the rollerball on the entire pot, the prosthetic fossa as direct full duration, so the five to 214 looks to be correct. However, with your doctor saying that he did. Really a tarp you might want To go back to him and see about what he was really intending to do here, is it just to stop for the gross hematuria? Or was he really working to treat the BPH and taking a little bit more of the prostate, intending to do a TRP, in which case, you do want to see that reflected in the operative notes so I can see why you're thrown off. It is one of those things that ultimately, when you look at it from a coding perspective, doesn't give you that extra fine feeling that in fact, they were focused on the BPH here it looks like kind of where you are that it was really focused more along the lines of obtaining the hemostasis because of the gross hematuria. So I double check with your physician, talked to him a little bit about whether or not that's what he intended to do. But 5221 for wood, wood. Fit roughly the definition of what you're doing. But again, important in in what he was intending to do here and expand that note to support what he was actually doing.
Scott 14:12
Ray anything.
Ray 14:15
Martin clear, if there was actually tissue removed or ablated to treat BPH, it would fit the tarp, but otherwise it would be a full duration.
Scott 14:27
All right. Very good. Anything else to add to this?
Mark 14:33
Nope. Nothing else. I think that's those are both good. Claire. All three were great questions. Thank you very much. Hopefully we got answers that give you enough to work with.
Scott 14:43
Alright.
Thanks for listening and please be on the lookout we are. We've opened up registration for our e&m live online workshop. So we're gonna have four workshops that are roughly going to be three hours each, that will We're going to really help you get prepared for e&m 2021 changes. So Mark was, you know, did a did a good job on breaking down the rules and what, what's changed and one of the things that has changed is increasing e&m reimbursement. However, if you don't really know, and don't really know the rules and how they've changed and that you're not prepared, then that might negatively affect you. So you need to or you might not take full advantage of what is changing in the new rules. So please make sure you're prepared. We do have any nm preparation checklist for you out on our website. So you can check that out. But we strongly encourage you to come join us on these workshops will really get you prepared. So thanks again for listening.
Mark 15:50
It's got one thing I think is you want to make a little bit clearer as the workshops or the are just this it's the same workshop at different times. So it's not a series of four, it's so we just had four different opportunities for everyone to join us. And we are going to really dive deeply on some of the nuances of these change the changes that are out there. And there's a few things that you know, as they change the rules that are going to make a difference. Some things that were fours are going to drop down to threes, and some things that were twos are going to jump up to threes, some threes are going to move to four. So it'll make a big difference. And then we've totally redesigned the Pocket Card and wall charts. So you'll need new pocket cards and wall charts too. So come join us for those. You know it and certainly you're going to look at what you need to do for your electronic medical record, which is why we're putting these in September and October. So you've got a little bit of time to make some changes to get ready. And we'll probably do a refactor In December of some type, just to make sure we've got everything covered in case, there are some crazy last minute changes from the final and the final rule which this year as you know is not going to come out until the first the last of November or the first of December. So we don't have a lot of time to react. It's gonna be a tight one this year.
Scott 17:25
And, and Mark did mentioned, you know, these are workshops, and we're diving deep. And one of the things it's not just your standard webinar where we're just going to be, you know, Mark's gonna be presenting for three hours, we're going to have physician, practicing urologist join us as well. And we're really going to do you know, a lot of different workshop breakouts. So we're going to use the Zoom rooms and it's going to be really interactive and a lot more. Hopefully more informative than just listening to three hour presentation. So So we really are trying to take advantage of, of the technology that we do have and that we are using given that we can't meet in person. So I think we've got some good things scheduled and you will is part of the workshop be receiving the Pocket Card and wall chart via mail so you will get a hard copy of that as well. So, anything to add?
No. Happy coding everybody. Thank you for listening to the Rogen coding and reimbursement podcast. We help urologists staff, economic practice efficiency, time and energy.
Special thanks to Carl Peters. For the music. You can find. Under his record label the T shirt. Special guests